Classification and anthropometric behavior of patients hospitalized in the pediatric service of the San Ignacio University Hospital during the months of June to October 2019
Main Article Content
Abstract
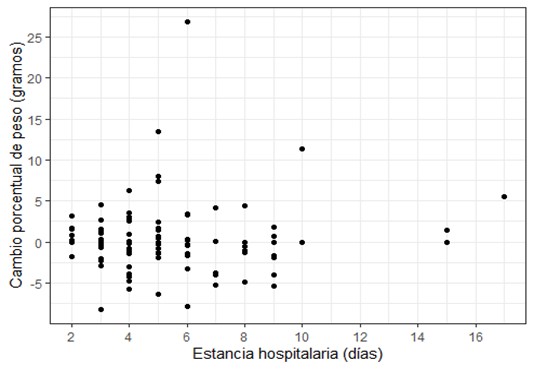
Introduction: Malnutrition is an imbalance between nutrient requirements and intake, which harms the organism and growth, increasing morbidity and mortality. The probability of developing nutritional deficiencies is greater during hospitalization, and clinical outcomes are poorer when this condition is not treated. Objective: To know the anthropometric behavior of patients from 1 month to 15 years old admitted to the San Ignacio University Hospital pediatric service in Bogotá, Colombia, in 4 months. Methods: A longitudinal and descriptive study in which five supervised and trained medical students took anthropometric measurements of hospitalized patients who met the inclusion criteria between June and October 2019. The variables were entered into a database daily, and their analysis was done with Stata 17. Results: Data from 100 children were obtained, the average age was 3.6 years, and most were hospitalized between 4 to 7 days. The most common diagnoses were pneumonia and asthmatic crisis. The population studied had a low frequency of obesity and overweight, and 44 % of the patients lost weight during hospitalization. 19 % of the children were admitted and discharged at risk of global malnutrition, 10 % with a diagnosis of global malnutrition, and at the end of hospitalization, the number of patients at risk of malnutrition increased by 6%. Conclusions: it is recommended to evaluate the nutritional risk of all patients admitted to the pediatric service regardless of the diagnosis, as well as to carry out an intrahospital anthropometric follow-up and manage those identified with alterations, ensuring their post-discharge surveillance.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Rinninella E, Ruggiero A, Maurizi P, Triarico S, Cintoni M, Mele MC. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. Eur Rev Med Pharmacol Sci. 2017;21(11):2690–701.
Aurangzeb B, Whitten KE, Harrison B, Mitchell M, Kepreotes H, Sidler M, et al. Prevalence of malnutrition and risk of under-nutrition in hospitalized children. Clin Nutr [Internet]. 2012;31(1):35–40. Available from: http://dx.doi.org/10.1016/j.clnu.2011.08.011. DOI: https://doi.org/10.1016/j.clnu.2011.08.011
Joosten KFM, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008;20(5):590–6. DOI: https://doi.org/10.1097/MOP.0b013e32830c6ede
Franco Londoño Á, Mejía López S. Factores de riesgo para malnutrición relacionados con conocimientos y prácticas de alimentación en preescolares de estrato bajo en Calarcá. Pract Pre- Sch Child Rev Gerenc Polit Salud. 2007;8(15)(15):77–90.
National Institute of Health of Colombia. Resolution Number 00002465 of 2016. Colomb Minist Heal Soc Prot [Internet]. 2016;47. Available from: https://www.icbf.gov.co/sites/default/files/resolucion_no._2465_del_14_de_junio_de_2016.pdf.
Beser OF, Cokugras FC, Erkan T, Kutlu T, Yagci R V., Ertem D, et al. Evaluation of malnutrition development risk in hospitalized children. Nutrition. 2018;48:40–7. DOI: https://doi.org/10.1016/j.nut.2017.10.020
Pacheco-Acosta JC, Gomez-Correa AC, Florez ID, Cortés JE, Velez D, Gomez J, et al. Incidence of nutrition deterioration in nonseriously ill hospitalized children younger than 5 years. Nutr Clin Pract. 2014;29(5):692–7. DOI: https://doi.org/10.1177/0884533614533122
Corkins MR. Why Is Diagnosing Pediatric Malnutrition Important? Nutr Clin Pract. 2017;32(1):15–8. DOI: https://doi.org/10.1177/0884533616678767
Rodríguez G, Vargas S, Ibáñez E, Matiz M, Jörgen-Overgaard H. Relación entre el estado nutricional y el ausentismo escolar en estudiantes de escuelas rurales. Rev Salud Pública [Internet]. 2015;17(6):861–73. Available from: https://revistas.unal.edu.co/index.php/revsaludpublica/article/view/48709/62625. DOI: https://doi.org/10.15446/rsap.v17n6.48709
Larson-Nath C, Goday P. Malnutrition in Children With Chronic Disease. Nutr Clin Pract. 2019;34(3):349–58. DOI: https://doi.org/10.1002/ncp.10274
Katoch OR. Determinants of malnutrition among children: A systematic review. Nutrition [Internet]. 2022;96:111565. Available from: https://doi.org/10.1016/j.nut.2021.111565. DOI: https://doi.org/10.1016/j.nut.2021.111565
López MTF, Baamil OF, Doldán CL, Alonso MLB, De Sas Prada MT, Labrador FL, et al. Prevalencia de desnutrición en pacientes hospitalizados no críticos. Nutr Hosp. 2014;30(6):1375–83.
Wonoputri N, Djais JTB, Rosalina I. Validity of Nutritional Screening Tools for Hospitalized Children. J Nutr Metab. 2014. DOI: https://doi.org/10.1155/2014/143649
Santafé Sánchez LR, Sánchez Rodríguez DA, Villegas Galarza AL, González-Correa CH. Estado nutricional en niños hospitalizados con diagnósticos mixtos en un hospital universitario de referencia en Manizales, Colombia. Nutr Hosp. 2012;27(5):1451–9.
Corkins MR, Griggs KC, Groh-Wargo S, Han-Markey TL, Helms RA, Muir L V., et al. Standards for nutrition support: Pediatric hospitalized patients. Nutr Clin Pract. 2013;28(2):263–76. DOI: https://doi.org/10.1177/0884533613475822
Mehta NM, Corkins MR, Lyman B, Malone A, Goday PS, Carney L, et al. Defining pediatric malnutrition: A paradigm shift toward etiology-related definitions. J Parenter Enter Nutr. 2013;37(4):460–81. DOI: https://doi.org/10.1177/0148607113479972
Quadros DRS, Kamenwa R, Akech S, Macharia WM. Hospital-acquired malnutrition in children at a tertiary care hospital. South African J Clin Nutr [Internet]. 2018;31(1):8–13. Available from: http://doi.org/10.1080/16070658.2017.1322825. DOI: https://doi.org/10.1080/16070658.2017.1322825
Rocha GA, Rocha EJM, Martins C V. The effects of hospitalization on the nutritional status of children. J Pediatr (Rio J). 2006;82(1):70–4. DOI: https://doi.org/10.2223/JPED.1440
Campanozzi A, Russo M, Catucci A, Rutigliano I, Canestrino G, Giardino I, et al. Hospital-acquired malnutrition in children with mild clinical conditions. Nutrition [Internet]. 2009;25(5):540–7. Available from: http://dx.doi.org/10.1016/j.nut.2008.11.026. DOI: https://doi.org/10.1016/j.nut.2008.11.026